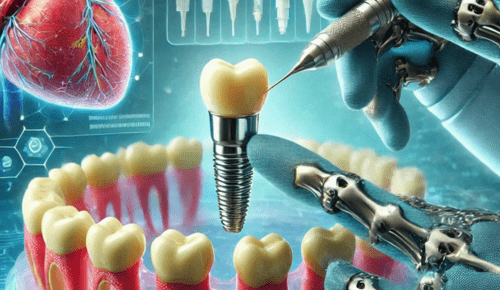
Stem cell-based therapies are a relatively young branch of science that employs a number of bioengineering strategies to promote reparative and regenerative actions in tissues. In the case of dental implants Oahu has provided the ability as to how the osseointegration process could be promoted by improving the interface between an implant and the bone.
This improvement can significantly increase the success rates of the implants, and provide a positive outcome for both patient and physician. Given its utility in accelerating the rates of tissue healing, regenerative medicine may be used to enhance the long-term success of dental implants.
What is the role of stem cells in implant integration?
Stem cells provide an ideal meaning in regenerative medicine for implant integration. Such cells can differentiate into other forms of tissues including soft body and bone tissues. Stem cells when used in the context of the anatomy surrounding the dental implant can be used to encourage faster bone regeneration and healing making the interface stronger with the dental implant. It can help to shorten the recovery period and increase the stability of the implant in the future, so it works better for patients.
What Is the Role of Platelet-Rich Plasma (PRP) in Endosseous Implant Success?
Another method/treatment within regenerative medicine is called Platelet-Rich Plasma or PRP therapy which helps in the healing. Concentrating the platelets within the patient’s blood, PRP gives a powerful focus on growth factors directing the healing of the injured tissue. Consequently, when used around these dental implants, the PRR can improve the formation of new bone and soft tissues around the implant thus improving integration. It has been observed through similar cases that PRP has the advantage of minimizing inflammation, reducing recovery period, and better long-term results in implant surgeries.
How do biomaterials support the Osseointegration of implants?
Biomaterials are designed to interface with the body therapeutically and to induce a response from the body such as tissue regeneration. Of the possibilities, hydroxyapatite or calcium phosphate can be used to coat the implant to raise the biocompatibility of the materials and therefore increase the bone formation around the implant. They provide the support necessary for these cells to attach to and thereby for new bone to grow around and incorporate with the implant. Thus, with the help of new materials used in implantology, practitioners can raise the chances of successful implantation and minimize the possibility of implant loss because of Sharpey’s fibers’ poor attachment.
What Are the Financial Consequences of Applying Regenerative Medicine in Implants?
Despite improving prosthetic dental implant surgery, regenerative medicine has its cost implications. Stem cells, PRP, growth factors, and biomaterials mean that the costs of treatment are generally higher. But these costs should be contrasted with the long-term advantages that may accrue from its use.
Better implant attachment results in decreased incidences of complications, the need for implant replacement, and enhanced patient satisfaction; factors that decrease overall costs for patients and dental professionals in the long term. However, better integration results in the fact that the number of additional visits is reduced; in turn, the financial aspect of the treatment is also maximized.
Conclusion
Regenerative medicine is a progressive area in dental implants, especially in relation to implant osseointegration. Treatments such as stem cell therapy, PRP, growth factors, and biomaterials can all improve the full healing process, which in turn will increase the long-term survival of implants. While these treatments may include extra costs, the financial return from lower risks expected by patients and improved results for doctors also justifies this plan. In conclusion, the principles of regenerative medicine will help to radically transform dentistry, and in particular, implantation techniques to improve implant bonding.
